MRI technology continues to improve with each new version in the market place. These improvements have allowed the imaging technology to better define the structures in the body. In the musculoskeletal system these technologies have allowed clinicians to identify injured tissues which may contribute to a patient’s painful presentation. MRIs have also been shown to...
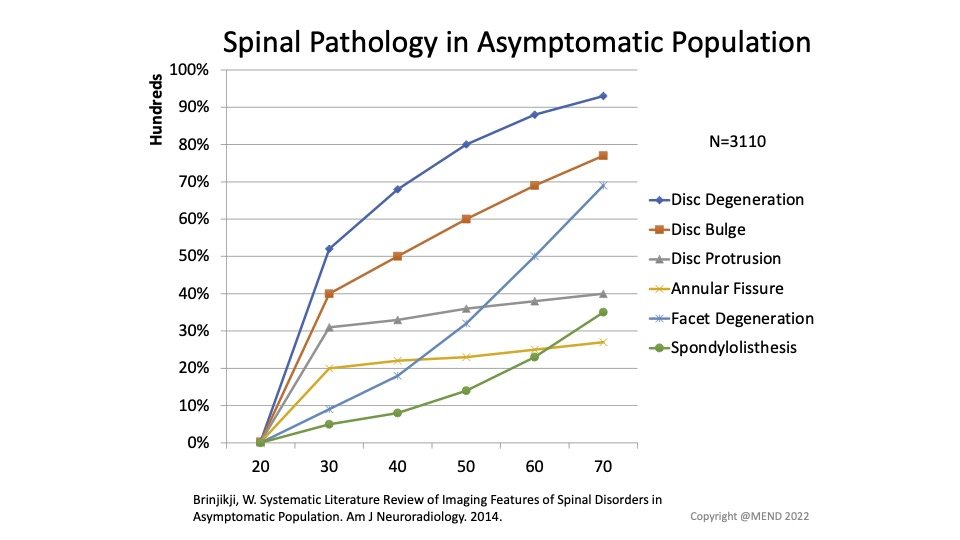
Low back pain is one of the most common conditions treated by physical therapists. Studies have shown that up to 90% of people without low back pain have findings on imaging like MRIs and X-rays (Brinjikji 2014). Because of this poor correlation between certain types of low back pain and imaging there can be more...
There is an old saying in medicine “the difference between pathology and pain is the patient”. In our Boulder Physical Therapy and Lafayette Physical Therapy clinics this is shown in the interpretation of MRI results. As these images have become more and more sensitive they rarely miss anything in the body, but often find pathology...
Our understanding of low back (lumbar) disc injuries and their influence on a patient’s pain and function has grown tremendously over the last couple of decades. Importantly, understanding the high prevalence of lumbar disc pathology on MRI imaging in asymptomatic healthy adults over the age of 30. These studies have given pause to clinicians who...
MRI technology continues to improve benefiting clinicians searching for serious pathology, but at a cost of identifying non serious pathology which may not be related to a patient’s clinic presentation. Initial imaging studies in the 1990s were conducted in the lumbar spine which identified a high percentage of structural changes including disc herniations and spinal...
Will My Disc Injury Heal Without Surgery?
August 13, 2020
In previous blogs we have discussed the limitations of imaging, including MRI, for musculoskeletal conditions including low back pain. The presence of pathology including disc herniations, nerve compression, arthritis, and degenerative disc disease increases with age in both pain free and painful individuals. The high degree of positive findings among asymptomatic individuals questions the ability...
Rates of hip arthroscopic procedure rates for labral tears and femoroacetabular impingement (FAI) have sky rocketed over in the last couple of decades secondary to more surgeons being trained in this area, as well as, a higher utilization of MRI testing in patients with hip pain. As we have discussed in prior blogs on imaging...
The old saying that you can’t unring a bell is true in imaging for musculoskeletal conditions. Most patients cannot unsee their MRI results despite improvements in their symptoms and activity level with Physical Therapy treatments. Once terms such as bulging or degeneration have been utilized to describe their spines they never regain full confidence in...
photo credit: radiopaedia.org Magnetic Resonance Images (MRI) have become increasingly sensitive to detecting abnormalities and pathologies in our bodies. As the technology has advanced radiologists are far less likely to miss an abnormality in the musculoskeletal system, but are more likely to find abnormalities that may or may not be causing a patient’s current symptoms....
Degenerative Disc Disease (DDD) is a commonly utilized “diagnostic” term given to patients frequently after neck and low back MRIs. It is hard to think of a more uninformed and harmful diagnosis in musculoskeletal medicine than DDD. Initially utilized to describe age related changes in the spinal structures secondary to aging, DDD continues to induce...