Are you wondering when it will happen to you? Not what , but when will you feel pain or develop an injury? Can you determine your injury risk? The answer is YES! There are screening tools that allow athletes to assess their injury risk. The Functional Movement Screen (FMS) is a valid indicator of injury risk among athletes. The FMS is a means of identifying your weak links and asymmetries in your basic functional movements.
As the triathlon season comes to a close, we finally have an opportunity to reflect on the season’s successes and create opportunities for improvement. During the offseason, we you are able to plan and prepare for the upcoming season. Prior research reports 10,000 athletes seek treatment for sports and exercise related injuries each day and over 7 million athletes receive medical attention over any 2 year span(2,3). In triathletes, up to 90% of individuals report at least one injury over the previous 1-2 seasons with the majority of these injuries occurring in the lower extremity(4). Unfortunately, the nature of these injuries leads to an inability to complete triathlon training in up to 75% of athletes causing an average loss of 2-3 months of training(5). Outside of traumatic events such as a bike collision, the vast majority of these injuries are diagnosed as overuse including achilles tendinopathy, medial tibial stress syndrome (shin splints), and plantar fasciitis, all which could have been prevented with a proper sport specific screening program and intervention.
Screening programs for triathletes should focus on known, modifiable intrinsic and extrinsic risk factors for injury. Intrinsic (individual) risk factors such as prior injury and supinated foot type, as well as, extrinsic (environment) risk factors including training volume (duration, intensity, frequency, and distance) and competition distance (Ironman) have been shown to increase the likelihood of future injury(6). Conversely, this research has demonstrated the presence of strength training, coach/club participation and medical team support have reduced an triathlete’s risk of future injury(7,8). Expert opinion suggests athletes should consider cross training, equipment fitting, reasonable training schedules and techniques, and pre-participation screenings to reduce future risk.
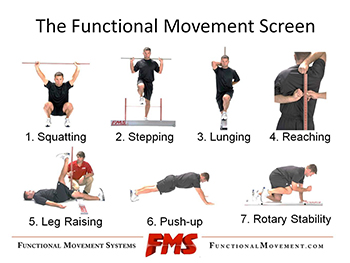
In our clinic’s experience, the utilization of The Functional Movement Screen (FMS) is an essential part of our pre-participation screening. The FMS consists of seven different functional movements that assess the following: trunk and core stability, neuromuscular coordination, asymmetry in movement, flexibility, acceleration, deceleration, and dynamic flexibility(10).
This component of our screen allows our Physical Therapists to objectively score and grade individuals for injury risk prior to participation as well as follow and reassess these at-risk individuals after Physical Therapy treatment is initiated.
Research has identified a score of 14/21 as an acceptable cut off for determining future injury risk. Athletes who score <14/21 are up to 11 times more likely to sustain an injury causing significant time away from training and competition(9). Lower scores may either reflect a current injury or a compensatory movement pattern, which will lead to a future injury. This data is then analyzed by the treating Physical Therapist to implement an intervention program consisting of corrective exercises that restore muscle balance and movement patterns, improve FMS scores, improve performance and reduce time away from their sport. These corrective exercises have been shown to improve FMS scores reducing time away from training and future injury risk(9,10).
Single plane exercises including running and cycling have been shown to develop asymmetry throughout the body and athletes with these imbalances often train around or neglect these weaknesses(11,12). The results of the FMS can be used to identify injury risk and to guide training programs.
Off seasons are an excellent time to recover from the season and address both nagging injuries as well as prevent future injury. The FMS is an integral part of any pre-participation examination and can quickly and effectively identify modifiable risk factors in athletes. For more information on the FMS or how Physical Therapy can assist in your training and performance contact the experts at MEND PT.
References
1. Dias Lopes, A. et al. What are the main running-related musculoskeletal injuries. Systematic Review. Sports Med. 2012;42(10):891-905.
2 National Center for Injury Prevention and Con- trol, Centers for Disease Control and Prevention. CDC Injury Research Agenda. Atlanta, GA: US Department of Health and Human Services; 2002.
3 Gotsch K, Annest JL, Holmgren P, Gilchrist J. Nonfatal sports- and recreation- related injuries treated in emergency departments—United States, July 2000–June 2001. MMWR Morb Mortal Wkly Rep. 2002;51(33):736-740.
4 O’Toole ML, Hiller WDB, Smith RA, et al. Overuse injuries in ultra endurance triathletes. Am J Sports Med 1989;17(4):514—8.
5 Vleck VE, Garbutt G. Injury and training characteristics of male elite, development squad, and club triathletes. Int J Sports Med 1998;19(1):38—42.
6 Gosling, C. Triathlon related musculoskeletal injuries. The status of injury prevention knowledge. J Science and Medicine in Sport. 2008. 11:396-406.
7 Egermann M, Brocal D, Lill CA, et al. Analysis of injuries in long-distance triathletes. Int J Sports Med 2003;24(4):271—6.
8 Aaltonen, S. Prevention of Sports Injuries. A systematic review of randomized controlled trials. Arch Phys Med Rehab. 2007. 167(1383-1396).
9 Chorba RS, Chorba DJ, Bouillon LE, Overmyer CA, Landis JA. Use of a Functional Movement Screening Tool to Determine Injury Risk in Female Collegiate Athletes. N Am J Sports Phys Ther. 2010; 5(2):47-54.
10 Peate WF, Bates G, Lunda K, Francis S, Bellamy K. Core strength: a new model for injury prediction and prevention. J Occup Med Toxicol. 2007; 2: 3.
11 Beckham, SG and Harper, M. Functional training: Fad or here to day? American college for Sports Medicine’s Health and Fitness Journal 14(6): 24-30, 2010.
12 Jaffe, L and Cook, G. One frame at a time. Training and Conditioning 16:8, 2006.